Advanced stem cell therapy to reduce keloid scars and restore healthy skin balance.
Keilods Removal
Struggling with raised, stubborn scars? Learn about cutting-edge treatments backed by science.
Our Mesenchymal Stem Cells Treatment targets excess collagen buildup at its source, reducing scar tissue while supporting healthy regeneration for smoother, stronger, and healthier skin.
How do Keloids Form?
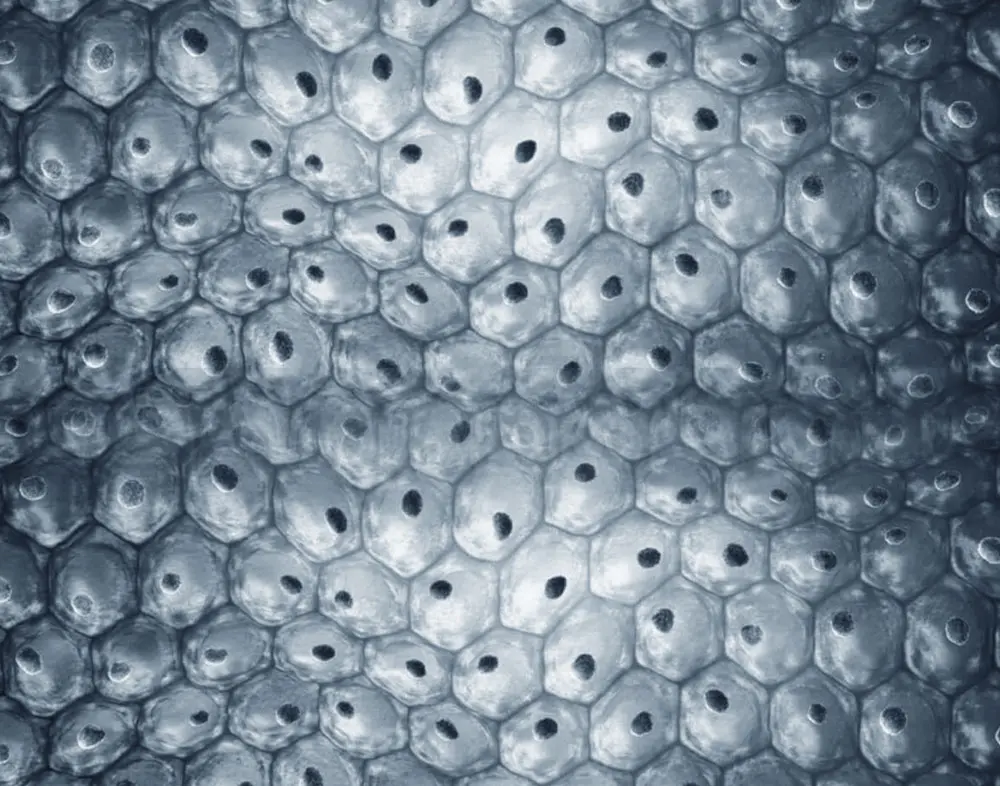
Keloids are the result of an abnormal wound healing process driven by an exaggerated immune response. When the skin is injured, the body naturally triggers inflammation to initiate tissue repair. However, in some individuals, this immune-mediated inflammatory response becomes excessive and prolonged. This chronic inflammation stimulates fibroblasts to overproduce collagen and extracellular matrix components beyond what is needed for normal healing. As a result, a dense, raised scar—known as a keloid—develops, often extending beyond the boundaries of the original injury. Keloid formation is therefore not simply a matter of scarring, but a dysregulated immune and inflammatory process that leads to pathological tissue remodeling.
Mesenchymal Stem Cells: The Most Effective Treatment for Keloids
Unlike conventional treatments that focus on removing the keloid or suppressing symptoms, Mesenchymal Stem Cells (MSCs) target the root cause of keloid formation: an abnormal immune response, chronic inflammation, and uncontrolled fibrosis.
MSCs are naturally immunomodulatory, meaning they regulate the immune system to prevent excessive or prolonged inflammatory reactions. They also possess strong anti-inflammatory and anti-fibrotic properties, which allow them to:

Calm the chronic inflammation that drives abnormal Scar formation
Inhibit the overactivation of Fibroblasts and excessive Collagen production

Restore balance to the wound-healing process
As a result, MSCs help reprogram the local tissue environment, preventing the recurrence of keloids and promoting healthy tissue regeneration instead of pathological scarring. Moreover, MSC-based therapies are completely non-invasive, usually administered through topical application or microinjections, and they do not damage the skin. They are biocompatible, with no side effects, and are safe for repeated use—even in sensitive or previously treated areas.
This makes MSCs the only truly effective and side-effect-free solution for managing keloids, particularly in patients where conventional treatments have failed or led to recurrence.
Why do Keloids return after removal?
Because keloids are driven by an underlying inflammatory and immune dysregulation, simply removing them surgically or with laser does not address the root cause. In fact, the act of removing the keloid creates a new injury to the skin, which can trigger the same inflammatory cascade – leading the body to form an identical keloid in the same area, often with the same or even greater volume and thickness. This is why recurrence after surgical or laser removal is very common, unless the immune-inflammatory response is properly modulated or suppressed during the healing process.
SURGICAL REMOVAL
Surgical removal of a keloid may seem like a straightforward solution, but in most cases, it is ineffective—and often counterproductive.
The act of excising a keloid creates a new skin injury: in individuals prone to keloid formation, the immune system reacts to injury with an exaggerated and prolonged inflammatory process. This leads to the formation of a new keloid scar—often as large or even larger than the original. Without addressing the underlying immune dysregulation and inflammation, surgical excision alone almost inevitably leads to recurrence.
Surgery is generally discouraged as a standalone treatment and is only considered when combined with adjuvant therapies (such as corticosteroid injections, silicone therapy, or radiation) aimed at modulating the wound healing response.
LASER ABLATION
Laser ablation—or resurfacing—may be effective for many types of scars, but it is generally ineffective for keloids. This is because keloids are not just superficial skin irregularities: they are the result of a deep, chronic inflammatory and immune-mediated process that affects the dermis and even subdermal layers.
When a laser is used to abrade or remove a keloid, it creates micro-injuries in the skin. In individuals prone to keloid formation, even these small injuries can reactivate the pathological wound-healing process—triggering excessive collagen production and leading to the formation of a new keloid, often identical or even worse than the original.
Without suppressing or modulating this underlying mechanism, laser treatment alone will not prevent recurrence—and in fact, may promote it.
The Stem Cell Source
Mesenchymal stem cells are the same regardless of whether they are derived from Adipose Tissue or Umbilical Cord Tissue. The only difference lies in their biological age, which reflects the age of the tissue of origin.
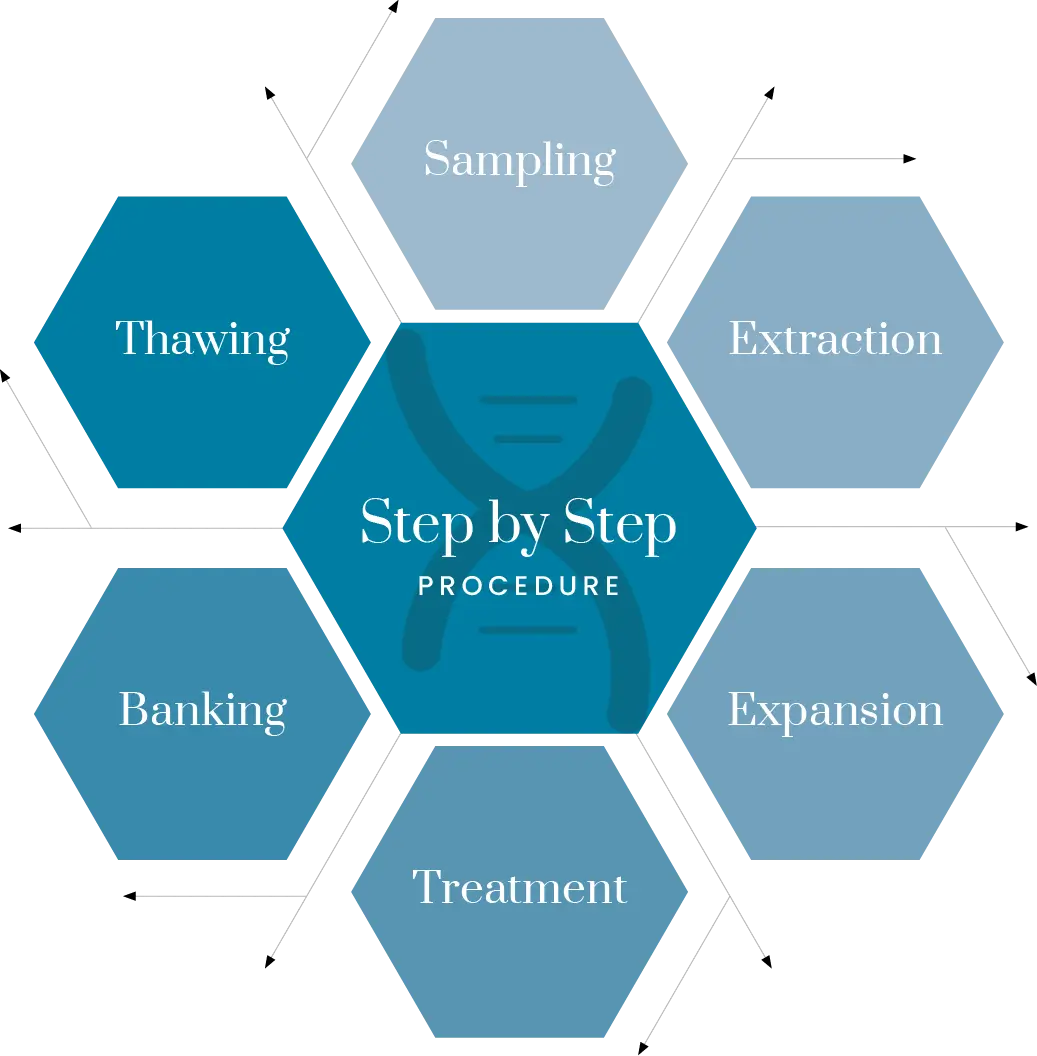
There are only 2 Mesenchymal Stem Cell Sources to treat Scars and Keilods:
Adipose Tissue Derived Stem Cells
The treatment requires a fat collection, stem cell extraction, and expansion. The entire process takes approximately 2–3 weeks.(*)

Umbilical Cord Tissue derived Stem Cells
The treatment does not require fat harvesting and can be performed within 2–3 days of the request.
(*) Therefore, from the moment of fat harvesting, a waiting period of 2–3 weeks is necessary before the treatment can be performed.
Let’s clarify with accurate information:
Stem Cells obtained from a fat sample require at least two weeks of processing before they can be used; otherwise, the treatment is ineffective and potentially harmful:
- Fat that is harvested and manipulated for use in the same session is both useless and harmful.
- There are no Stem Cells in the blood, so treatments claiming to use stem cells extracted from blood are not scientifically valid. The Stem Cells used to treat hematological diseases are found in the bone marrow, not in the blood.
- The hematopoietic stem cells found in umbilical cord blood are useful for treating blood disorders, but not for counteracting the aging processes of the human body
What to Expect from Mesenchymal Stem Cell (MSC) Treatment for Keloids Removal
Expanded MSC therapy—administered via injection or applied topically in controlled conditions—has consistently shown scar regression, improved tissue structure, and excellent safety in preclinical studies and early human trials. It represents the most promising, mechanism-driven approaches for keloid treatment.
MACROSCOPIC
IMPROVEMENT
MSC significantly reduced scar thickness and pale appearance, yielding smoother, flattened, and more visually acceptable scars with no reported adverse events.
HISTOLOGICAL & TISSUE-LEVEL BENEFITS
MSC significantly reduced scar thickness and pale appearance, yielding smoother, flattened, and more visually acceptable scars with no reported adverse events.
ANTI-INFLAMMATORY AND IMMUNOMODULATORY EFFECTS
MSCs shift macrophages from a pro-inflammatory M1 phenotype to anti-inflammatory M2, calming the excessive inflammatory response at the core of keloid pathogenesis.(*)
(*) Conditioned media from human adipose-derived MSCs suppressed fibrotic gene expression, reduced fibroblast proliferation and migration, and diminished angiogenesis in explant models.
Expected Result
Experience the regenerative power of stem cells to naturally reduce keloid scars and restore smoother, healthier skin.
- Scar Appearance
Thinning, flattening, normalization of texture or color - Tissue Composition
Less disorganized collagen, fewer myofibroblasts.
- Inflammation
Reduced chronic inflammation via macrophage modulation. - Side Effects
None reported in current research.
Ready to Take the Next Step?
Your journey to better health starts with a simple conversation
Our team of medical experts and dedicated patient coordinators is here to guide you every step of the way. From your initial consultation to post-treatment follow-up, we provide personalized support tailored to your unique needs. Schedule a free consultation today and discover how our advanced treatments can help you achieve your health goals.
