Pro-inflammatory Cytokine Monitoring Test
CYTOBALANCE
A pioneering test designed to reveal the invisible signals of inflammation before they compromise health
CYTOBALANCE by Bioscience Institute offers an advanced approach to monitor inflammation markers and detect silent inflammatory processes before they impact health.
This innovative program measures pro-inflammatory cytokines through a simple blood test, helping identify early signs of low-grade chronic inflammation — a condition increasingly recognized as a key driver of aging and chronic disease.
What is Inflammation?
Inflammation is a natural defense mechanism activated by the body to combat infection and tissue damage.
However, not all inflammation is caused by pathogens or trauma. In many individuals, especially with age, non-infectious low-grade inflammation can develop silently, without pain, redness, or swelling.
Maintaining cytokine levels within a balanced range can significantly reduce the risk of chronic conditions associated with this “silent” inflammation.
Chronic Low-Grade Inflammation
Persistent, low-intensity inflammation is one of the main contributors to aging-related diseases such as atherosclerosis, Alzheimer’s, Parkinson’s, type 2 diabetes, and several cancers.
Known as chronic low-grade inflammation, this process may not cause immediate symptoms, yet it gradually impairs physiological functions and accelerates cellular aging. Managing and monitoring it is key to preserving long-term health and longevity.
Inflammaging
Inflammaging describes the chronic, systemic inflammation that naturally develops with age.
It results from an accumulation of molecular and cellular debris, oxidative stress, and impaired immune regulation.
While initially adaptive, this state eventually becomes harmful, leading to a progressive decline in tissue function. Understanding inflammaging allows early lifestyle interventions that can help preserve immune balance.
Metaflammation
Metaflammation, or metabolic inflammation, occurs when excessive nutrient intake or poor dietary habits stimulate chronic inflammatory responses.
This process links obesity, insulin resistance, and type 2 diabetes to inflammatory pathways.
Monitoring cytokine levels can help detect early metabolic imbalances and guide corrective dietary and lifestyle choices.
Molecules Involved in Inflammation
Inflammatory processes are regulated by a complex network of signaling molecules known as cytokines.
These proteins mediate communication between immune cells and coordinate the body’s response to infections, tissue damage, and cellular stress.
Among the most important pro-inflammatory cytokines are interleukins such as IL-2, IL-4, IL-5, IL-6, IL-9, IL-10, IL-12, and IL-17A, as well as GM-CSF (Granulocyte-Macrophage Colony-Stimulating Factor), TNF-α (Tumor Necrosis Factor-α), and interferons (IFN-α and IFN-γ).
These molecules stimulate immune activation, regulate cell proliferation, and influence metabolic and vascular functions.
Another key marker is C-reactive protein (CRP) — a molecule produced by the liver under the stimulation of cytokines such as IL-6.
Even mild increases in CRP concentrations are considered a reliable indicator of chronic low-grade inflammation, making it an essential biomarker for preventive and longevity-oriented medicine.
By measuring cytokine and CRP levels together, it becomes possible to obtain a comprehensive view of the body’s inflammatory status — a valuable step for identifying early imbalances before they manifest as clinical disease.
Why Monitor Pro-Inflammatory Cytokines?
Chronic inflammation often progresses silently, without the visible symptoms typical of acute inflammation.
Detecting elevated cytokines or CRP levels can reveal an underlying inflammatory state that would otherwise remain unnoticed.
The CYTOBALANCE test allows the monitoring of 9 inflammation markers through a simple blood draw.
Abnormal results indicate a possible low-grade inflammatory condition and the need for preventive strategies to restore balance.
| PCR |
|
|---|---|
| TNF-α |
|
| IFN-γ |
|
| IL-2 |
|
| IL-4 |
|
| IL-6 |
|
| IL-10 |
|
| IL-12 |
|
| IL-17A |
|
Taking Action
When a low-grade inflammatory state is detected, simple lifestyle modifications can make a measurable difference:
- Adopting a balanced, anti-inflammatory diet
- Managing stress effectively
- Reducing exposure to pro-inflammatory substances (tobacco, alcohol, hormones, toxins)
- Supporting immune balance with targeted food supplements under expert guidance
Additional analyses — such as microbiome testing or genomic instability analysis — can provide deeper insight into the causes and consequences of chronic inflammation.
Cytokines and Health
Pro-inflammatory cytokines regulate immune and inflammatory responses.
When their production is temporary, they support healing and defense.
When sustained, they contribute to tissue damage and disease progression.
High cytokine and CRP levels are correlated with a greater risk of cardiovascular disease and cancer, including colorectal and breast cancer.
Monitoring these markers enables early preventive action and supports personalized longevity strategies.
Clinical Indications for the CYTOBALANCE Test
CYTOBALANCE is designed for anyone who wishes to evaluate or monitor inflammation levels — even in the absence of symptoms.
It is particularly recommended:
- During aging, to detect and manage inflammaging
- In high-stress conditions
- For individuals with unbalanced diets or metabolic disorders
- In cases of smoking or exposure to toxins
- For those with gut dysbiosis, which is often linked to increased cytokine production
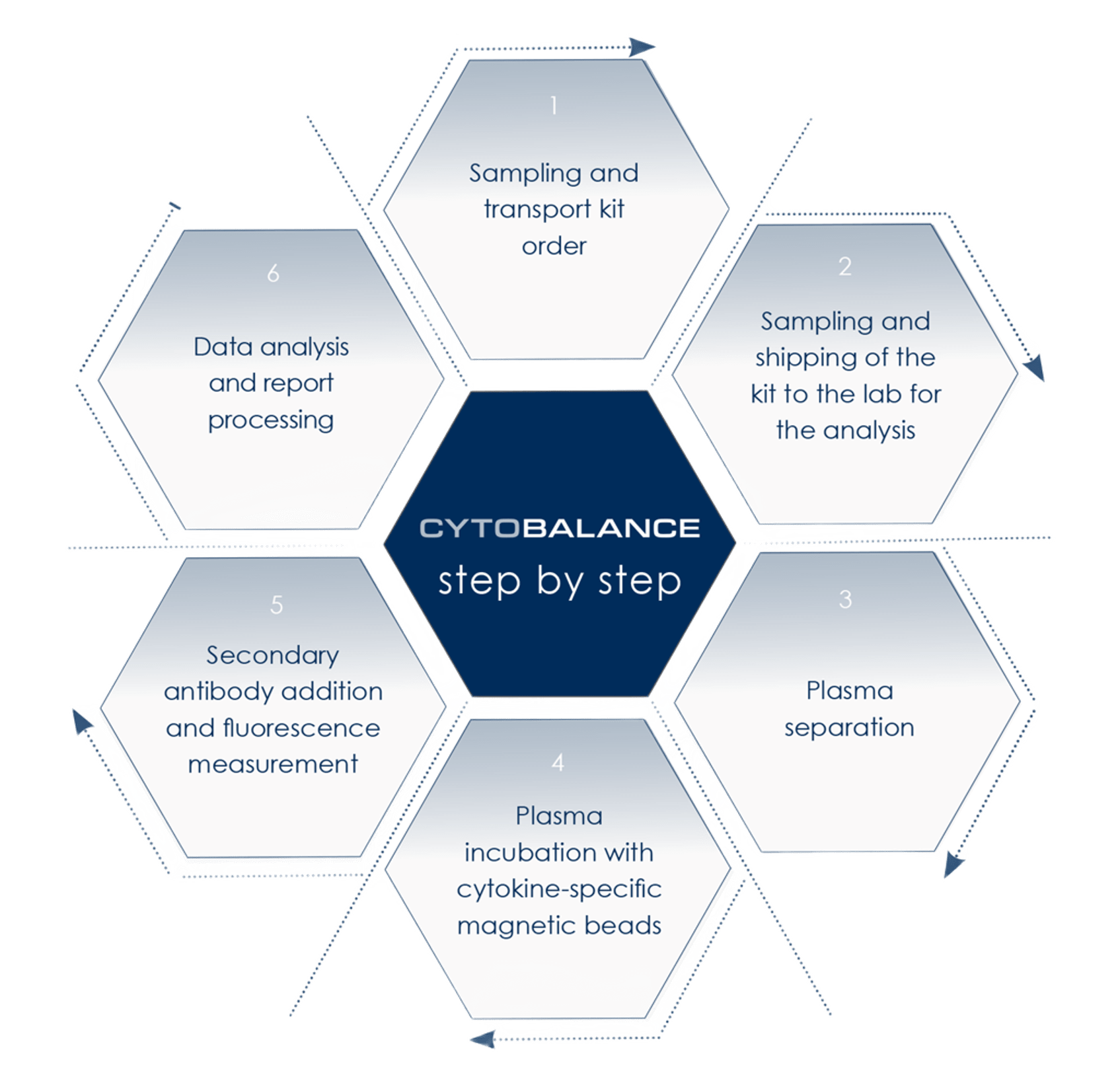
How the Test Works
The CYTOBALANCE test requires only a simple blood sample, collected using the dedicated sampling kit provided by the Bioscience Institute.
After the sample is taken, it is shipped to the Institute’s specialized laboratories using the temperature-controlled transport system included in the kit to ensure sample integrity.
Once received, the laboratory workflow follows a series of validated steps designed to precisely quantify inflammatory biomarkers:
- Sample processing and plasma separation — the plasma is isolated from the blood sample to allow targeted analysis.
- Plasma incubation with cytokine-specific magnetic beads — this phase enables the capture of pro-inflammatory cytokines and related molecules.
- Secondary antibody addition and fluorescence measurement — cytokine levels are detected using fluorescence-based immunoassays, ensuring high analytical sensitivity and specificity.
- Data analysis and report generation — the results are processed through advanced bioinformatic systems to obtain a complete cytokine profile, including CRP (C-reactive protein) quantification.
The resulting inflammation profile does not represent a clinical diagnosis but provides a powerful tool for prevention and personalized health optimization.
Results are interpreted by qualified medical specialists, who provide tailored recommendations for lifestyle, dietary habits, and, if appropriate, the use of targeted food supplements to help counteract low-grade chronic inflammation.
Follow-up testing may be advised based on individual results, medical history, and overall health objectives to monitor progress over time and evaluate the effectiveness of corrective strategies.
In-depth Information
Would you like to explore further or learn more? Access comprehensive explanations by expanding the sections below.
CHRONIC INFLAMMATION AND TUMORS
The link between inflammation and tumors depends on two different phenomena. On the one hand, genes involved in the development of cancer can stimulate inflammatory processes. On the other hand, inflammation increases the risk of cancer by suppressing antitumor immune responses and creating conditions that favor the accumulation of mutations, the growth and survival of tumor cells, the formation of blood vessels that nourish the tumor, the ability of tumor mass to invade surrounding tissues and to stimulate metastases.
The analysis of the inflammation levels enables the identification of situations of increased risk and the implementation of strategies to counter the increase in pro-inflammatory molecules.
The association between inflammation and cancers
The link between inflammation and tumors depends on two different phenomena. On the one hand, genes involved in the development of cancer can stimulate inflammatory processes. On the other hand, inflammation increases the risk of cancer by suppressing antitumor immune responses and creating conditions that favor the accumulation of mutations, the growth and survival of tumor cells, the formation of blood vessels that nourish the tumor, the ability of tumor mass to invade surrounding tissues and to stimulate metastases.
The mechanisms involved depend on the formation of reactive oxygen (ROS) and nitrogen (RNS) species which:
- alter DNA, proteins, and lipids;
- they also damage stem cells, favoring the development of particularly aggressive forms of cancer;
- cause a particular modification of the genome, demethylation, thus promoting another phenomenon associated with the development of cancer: genomic instability.
Furthermore, inflammation can reduce the expression of tumor suppressor genes and other molecules (microRNAs) that can block the development of tumors.
The markers of inflammation in tumors
Several molecules associated with inflammation are also associated with tumors. In particular, both tumor cells and those surrounding the tumor produce proinflammatory cytokines such as Tumor Necrosis Factor α (TNF-α), a molecule synthesized in the initial stages of the inflammatory response that also plays an important role in the maintenance of inflammation. TNF-α is involved in the mechanisms that regulate tumor growth and their ability to invade tissues and produce metastases.
In turn, proinflammatory cytokines regulate the production of C reactive protein (CRP). Its levels increase rapidly in case of inflammation and are associated with both tumor progression and reduced survival in the presence of various cancers (esophagus, stomach, colorectal, liver, pancreas, and ovary). Elevated CRP concentrations are associated with an increased risk of developing cancer (for example, colorectal or breast cancer) and increased colorectal cancer mortality.
When to analyze inflammation levels
CYTOBALANCE, the analysis of chronic inflammation levels by the Bioscience Institute, is specified in all cases in which it is desired to control the risk factors for the development of tumors through active primary prevention. Suitable for all healthy and asymptomatic individuals, it is particularly useful in the presence of an increased risk of inflammatory phenomena, such as for example:
- during aging
- in case of genetic predisposition to the development of tumors
- in case of exposure to cigarette smoke
- if you live in polluted environments
- when taking hormone-based therapies
- in case of high stress
- in case of unbalanced diet, overweight and obesity
- in case of intestinal dysbiosis (alterations of the intestinal bacterial flora)
INFLAMMAGING AND GUT MICROBIOTA
The population of microbes living in the gut (the gut microbiota) performs many beneficial functions. If altered, however, it can contribute to the development of inflammatory phenomena which, silently, increase the risks to health. Even the simple fact of aging can be associated with alterations in the microbiota (dysbiosis) capable of triggering inflammation. Precisely because it is associated with aging, this phenomenon is known as inflammaging.
Analyzing the inflammaging levels enables the evaluation of the consequences of intestinal dysbiosis and actions to be taken in a targeted way to fight the effects of the alteration of the microbiota.
Inflammaging
Over the course of life, a series of internal and external factors to the organism activate innate immunity, triggering inflammation and a metabolic response. This response is a defense mechanism and until middle age it is essential for the survival of the organism. However, aging is often associated with an increase in the inflammatory response, which can even become chronic and harmful. Furthermore, as we age, the ability to resolve inflammation decreases.
The chronic low-grade inflammation that accompanies aging is mainly associated with signals from within the organism, such as the presence of cellular debris or oxidized proteins and the accumulation of senescent cells. However, external factors such as stress or the microbiota also contribute.
The microbiota in inflammaging
Intestinal dysbiosis can contribute to both inducing inflammaging and maintaining it. In many cases their appearance depends on lifestyle, for example from the intake of drugs or from dietary changes typical of aging, in particular:
- from an increase in sugar consumption
- from an increase in fat consumption
- from a reduction of foods of plant origin
- by reducing the consumption of healthy foods
- by reducing the variety of foods
These dysbioses are responsible for variations in the short-chain fatty acids levels normally produced by the microbiota. In addition, they can cause nervous system degeneration associated with the intestine and alterations in intestinal motility, can reduce the intestinal barrier and increase the permeability of the intestine, resulting in an increase in the molecules that control inflammation (proinflammatory cytokines). Molecules of bacterial origin can pass into the blood, activating the immune system cells involved in atherosclerosis and stimulating the production of the beta-amyloid protein involved in Alzheimer’s disease.
When to analyze inflammaging associated with intestinal dysbiosis
Inflammaging can be analyzed with CYTOBALANCE, the test that monitors inflammatory cytokine levels developed by the Bioscience Institute.
The analysis is indicated in all cases in which intestinal dysbiosis is suspected or detected that could promote or feed the inflammatory condition typically associated with aging.
INFLAMMATION AND NUTRITION
The information provided by MyCarrier gains its true value through accurate interpretation.
Genetic counseling helps couples understand the results in the context of their personal and family medical history.
Counselors guide patients through risk assessment, explain inheritance probabilities, and discuss possible next steps, supporting informed, confident, and responsible reproductive choices.
INFLAMMATION AND MITOCHONDRIAL DNA
The information provided by MyCarrier gains its true value through accurate interpretation.
Genetic counseling helps couples understand the results in the context of their personal and family medical history.
Counselors guide patients through risk assessment, explain inheritance probabilities, and discuss possible next steps, supporting informed, confident, and responsible reproductive choices.
Ready to Take the Next Step?
Your path to better long-term health starts with understanding what’s happening inside your body.
Our specialists and scientific advisors are here to guide you from test selection to result interpretation, offering clear insights into your microbiome balance, chronic inflammation markers, genetic predispositions, and more. We provide personalized support tailored to your wellness goals.
Book your free consultation today and discover how our advanced molecular tests can help you take control of your health with confidence and clarity.
