Complete and accurate non-invasive prenatal screening test
ULTRANIPT
ULTRANIPT® is the most comprehensive and accurate non-invasive cell-free DNA prenatal screening test for fetal chromosomal abnormalities.
ULTRANIPT® test can detect not only 118 chromosomal abnormalities but also provide a clinical interpretation.
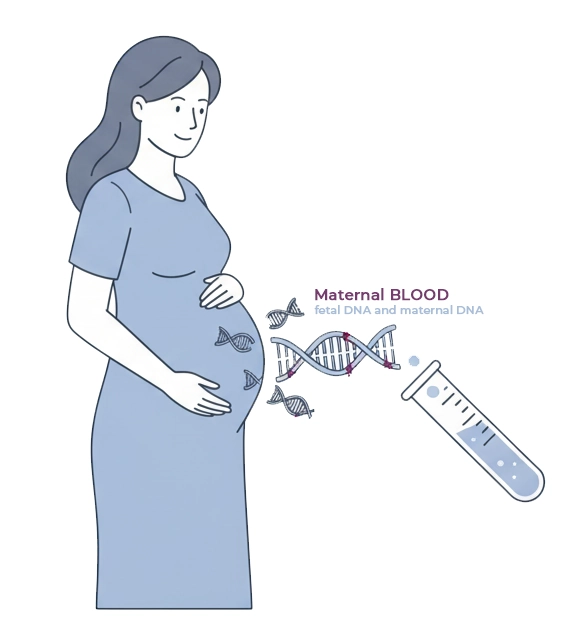
ULTRANIPT® test is performed on a maternal blood sample collected from the tenth week of gestation, when small fragments of fetal DNA circulating in maternal plasma can be analyzed to assess the presence of chromosomal abnormalities. The DNA is sequenced and analyzed using specific algorithms that enable the detection of chromosomal abnormalities across the entire genome.
Unlike the “targeted sequencing” methods used for some older-generation NIPT tests, or other cost-effective solutions lacking adequate clinical validation, the ULTRANIPT® methodology, through whole-genome analysis and advanced bioinformatics analyses, provides highly accurate results and a broader range of detectable abnormalities: trisomies, sex chromosome aneuploidies, and deletion/duplication syndromes affecting the entire chromosome set.
The introduction of new quality procedures and new bioinformatics algorithms has made ULTRANIPT® even more reliable and has allowed the indications to be extended to include twin pregnancies.
What ULTRANIPT test evaluates
The ULTRANIPT® test is offered in 5 analysis options, with increasing levels of detail:
| Detectable Syndromes | ULTRANIPT DG | ULTRANIPT 2.0 | ULTRANIPT WIDE | OMNIPT 3.0 | OMNIPT WIDE |
|---|---|---|---|---|---|
| Down Syndrome (T21) | ✔ | ✔ | ✔ | ✔ | ✔ |
| Edwards Syndrome (T18) | ✔ | ✔ | ✔ | ✔ | ✔ |
| Patau Syndrome (T13) | ✔ | ✔ | ✔ | ✔ | ✔ |
| Monosomy X * | ✔ | ✔ | ✔ | ✔ | ✔ |
| Klinefelter Syndrome (XXY) * | ✔ | ✔ | ✔ | ✔ | ✔ |
| Jacobs Syndrome (XYY) * | ✔ | ✔ | ✔ | ✔ | ✔ |
| Triple X Syndrome (XXX) * | ✔ | ✔ | ✔ | ✔ | ✔ |
| DiGeorge Syndrome | ✔ | ✔ | ✔ | ✔ | ✔ |
| DiGeorge Syndrome Type 2 | ✔ | ✔ | ✔ | ✔ | ✔ |
| 92 microdeletion / microduplication syndromes | ✘ | ✔ | ✔ | ✔ | ✔ |
| Rare autosomal aneuploidies | ✘ | ✔ | ✔ | ✔ | ✔ |
| Deletions / duplications on all chromosomes | ✘ | ✘ | ✔ | ✘ | ✔ |
| 202 de novo monogenic disorders | ✘ | ✘ | ✘ | ✔ | ✔ |
| Fetal sex | ✔ | ✔ | ✔ | ✔ | ✔ |
(*) not available for twin pregnancies
OMNIPT
The OMNIPT test includes ULTRANIPT (2.0 or WIDE) and can detect 202 dominant de novo monogenic disorders with an accuracy greater than 99%.
These are conditions caused by mutations in a single gene that appear for the first time in the family. It has been observed that de novo mutations occur more frequently in children of older couples, especially from the paternal side.
WIDE Option
The WIDE option includes the detection of deletions and duplications in all chromosomes, even if not included in the main panel and not associated with known syndromes, with the possibility of detecting anomalies larger than 5 Mb. In this case, the bioinformatic analysis may detect anomalies for which clinical interpretation is not available.
How ULTRANIPT® test is performed
By contacting Bioscience Institute filling out the ULTRANIPT ® request form, it is possible to receive all preliminary information (timelines, execution procedures, etc.) as well as details on the nearest affiliated centers where the test can be performed.
The maternal peripheral blood sample required for the ULTRANIPT® test is approximately 8 ml.
ULTRANIPT® test can be performed from the 10th week of gestation using the CE-IVD certified collection tube provided in the sampling and transport kit.
Samples are sent to the Bioscience laboratories, where the blood arrives inside an isothermal kit designed for the transport of Category B biological substances, in compliance with UN3373 regulations.
The most extensive clinical validation in the world
ULTRANIPT boasts the largest study ever published regarding a prenatal screening test based on fetal DNA. The study verified the accuracy of the results of 112,669 tests using diagnostic methods. The data confirmed the test’s ability to detect Trisomies 21, 18, and 13 with a sensitivity of 99.17%, 98.24%, and 100%, respectively, and a false-positive rate of less than 0.05%.
| Syndrome | Sensitivity* | Specificity** |
|---|---|---|
| T21 | 99.17% | 99.95% |
| T18 | 98.24% | 99.95% |
| T13 | >99.9% | 99.96% |
| Sex chromosome aneuploidies | >99.6% | >99.8% |
| Deletions Duplications | >10Mb | >99% |
| <10Mb | >99% | |
| De novo monogenic diseases | >99% | >99% |
| Fetal sex | >99% | >99% |
IN PREGNANT WOMEN UNDER 40 YEARS OF AGE
Positive Predictive Value for the Most Common Deletion Syndromes
| Syndromes | Incidence | PPV | PPV of other tests |
|---|---|---|---|
| DiGeorge Syndrome | 1/4000-1/10000 | 80.6% | 53% |
| Prader-Willi/Angelman Syndrome | PW:1/10000-1/30000 A:1/12000-1/20000 |
27.8% | 5% / 10% |
| Cri-du-chat Syndrome | 1/15000-1/50000 | 21.4% | 2-5% |
| 1p36 Deletion Syndrome | 1/5000-1/10000 | 10.0% | 7-17% |
| 18q Deletion Syndrome | 1/10000 | 66.7% | Data not available |
| 18p Deletion Syndrome | 1/50000 | 50.0% | Data not available |
| Wolf-Hirschhorn Syndrome | 1/20000-1/50000 | 60.0% | Data not available |
| 9p Deletion Syndrome | 1/50000 | 75.0% | Data not available |
| Smith-Magenis Syndrome | 1/15000-1/25000 | 66.7% | Data not available |
Data obtained from the review and follow-up of positive results from 210,217 tests.
GUARANTEE OF RELIABILITY
The guarantee of reliability, derived from the largest case study in the world (over 16 million tests performed), has made it possible for every pregnant woman who requests it to access a free insurance policy. Compensation may be available if certain aneuploidies are not detected. In cases of high risk, free genetic counseling and/or a contribution towards the cost of further diagnostic testing are available. **
(**) Insurance, compensation, and reimbursements are subject to limitations. For further details, please call us before undergoing the test.
Why choose ULTRANIPT® test
Discover the advantages of the prenatal test offered by Bioscience Institute
ULTRANIPT® test is a next-generation prenatal test that provides essential information about the genetic health of the fetus, with no risk to the mother or baby throughout the entire pregnancy.
ULTRANIPT® is the most validated and accurate cell-free DNA prenatal screening test for the evaluation of fetal abnormalities. It can detect up to 320 chromosomal abnormalities and monogenic disorders (OMNIPT), with the corresponding clinical interpretation. DNA is sequenced at high resolution (double that of other sequencing platforms) and analyzed using specific algorithms that enable the detection of genome-wide anomalies, even microscopic ones (up to 1 MB), while maintaining high reliability of results.
The introduction of new quality procedures and new bioinformatics algorithms has made ULTRANIPT® even more reliable and has allowed the indications to be extended to include twin pregnancies.
Through a simple maternal blood draw, it delivers rapid and highly accurate results. Here are the main advantages:
- A study of 146,958 pregnant women makes ULTRANIPT® the most validated fetal DNA test.
- ULTRANIPT 2.0 can detect 118 chromosomal abnormalities.
- With the WIDE option, it is possible to detect abnormalities affecting all chromosomes.
- With the OMNIPT test, the search can be extended to 202 monogenic diseases.
- The new fetal fraction enrichment procedure increases the test’s accuracy.
- New algorithms improve the PPV for all syndromes, even microscopic ones (up to 1 Mb).
- Thanks to a reading depth of 800X, OMNIPT’s sensitivity and specificity are greater than 99%.
- Rare syndromes were selected from those with a clear clinical picture documented in the literature.
- The clinical interpretation provided in the case of detected abnormalities facilitates counseling.
When is the ULTRANIPT test recommended?
Singleton pregnancies conceived through assisted reproduction (including egg donation)
Twin pregnancies conceived through assisted reproduction (including egg donation)
IMPORTANT NOTICE
The OMNIPT option is indicated in single pregnancies, with the exception of those resulting from heterologous assisted fertilization.
In-depth Information
Would you like to explore further or learn more? Access comprehensive explanations by expanding the sections below.
Information about ULTRANIPT test results
The maternal peripheral blood sample required for the ULTRANIPT test can be performed starting from the 10th week of gestation (up to the 24th week) using the CE-IVD certified tubes provided in the collection and transport kit. The collected blood is transported in an insulated kit for category B biological material, in compliance with the UN3373 regulation.
Results are available in approximately 7 working days (14 for monogenic disorders). This is a complex analysis for which we have always prioritized quality over speed: this is because we value accurate results more than results received 1 or 2 days early.
It is important to note that processing times may vary: the analysis involves a series of rigorous quality controls to ensure the reliability of the results, including verification of the amount of fetal DNA present in the blood sample, which varies from pregnant woman to pregnant woman. In some cases, due to a low fetal DNA content, it is necessary to repeat the analysis and/or blood sampling. If the test needs to be repeated due to a low fetal DNA concentration in the maternal blood, the repeat will be free of charge.
Monogenic diseases detectable with the OMNIPT option
SOME OF THE DETECTABLE DISEASES

MONOGENIC
DISEASES
Syndromes detectable with ULTRANIPT 2.0
| 1p36 Deletion Syndrome | 5p Duplication | 10q26 Deletion Syndrome | 15q26 Chromosome Overgrowth Syndrome |
| 1q41-q42 Deletion Syndrome | 6pter-p24 Deletion Syndrome | 10p12-p11 Deletion Syndrome | 16p12.2-p11.2 Deletion Syndrome |
| 1p32-p31 Deletion Syndrome | 6q24-q25 Deletion Syndrome | 10p Duplication | 16p12.2-p11.2 Duplication Syndrome |
| 2p16.1-p15 Deletion Syndrome | 6q11-q14 Deletion Syndrome | 11p13 Deletion Syndrome | 16p13.3 Deletion Syndrome |
| 2q33.1 Deletion Syndrome | 6p Deletion | 11p11.2 Deletion Syndrome | 16p13.3 Duplication Syndrome |
| 2q31.1 Duplication Syndrome | 6q15-q23 Deletion Syndrome | Jacobsen Syndrome | 16q Proximal Duplication Syndrome |
| 2q37 Deletion Syndrome | 6q25-qter Deletion Syndrome | 11q23 Deletion Syndrome | Smith-Magenis Syndrome |
| 2q31.1 Microdeletion Syndrome | 6q26-q27 Deletion Syndrome | 12q14 Microdeletion Syndrome | 17p13.3 Deletion Syndrome |
| 2q Duplication Syndrome | 7q Deletion | 12p12.1 Microdeletion Syndrome | Potocki-Lupski Syndrome |
| 3pter-p25 Deletion Syndrome | 7q11.23 Deletion Syndrome | 12p Duplication | 17p13.3 Duplication Syndrome |
| Dandy-Walker Syndrome | 7q21-q32 Deletion | 13q14 Deletion Syndrome | Yuan-Harel-Lupski Syndrome |
| 3q13.31 Deletion Syndrome | 7q31-q32 Deletion | 13q Distal Deletion | 17p Duplication |
| 3p Distal Duplication Syndrome | 8p23.1 Deletion Syndrome | 14q11-q22 Deletion Syndrome | 18p Deletion Syndrome |
| 3q Duplication Syndrome | 8p23.1 Duplication Syndrome | 14q22 Deletion Syndrome | 18q Distal Deletion Syndrome |
| 4p16.3 Deletion Syndrome | Langer-Giedion Syndrome | 14q Proximal Deletion | Alagille Syndrome 1 |
| 4q21 Deletion Syndrome | 8q22.1 Deletion Syndrome | 14q Duplication | 20p Duplication |
| 4p Duplication | 8q22.1 Duplication Syndrome | Angelman Syndrome | 21q22 Deletion |
| 4q Distal Duplication | 8p Duplication | Prader-Willi Syndrome | 22q11.2 Deletion Syndrome (includes DiGeorge)** |
| 4q Distal Deletion | 8q Duplication | 15q Distal Deletion | Xp11.23-p11.22 Duplication Syndrome |
| Cri-du-Chat Syndrome | 9p Deletion Syndrome | 15q26-qter Deletion Syndrome | Xp21 Deletion Syndrome |
| 5q14.3 Deletion Syndrome | 9p Duplication | Levy-Shanske Syndrome | Xq27.3-q28 Duplication Syndrome |
| 5q12 Deletion Syndrome | DiGeorge Syndrome 2** | 15q14 Deletion Syndrome | Xq21 Deletion Syndrome |
| 5p13 Duplication Syndrome | 10q22.3-q23.2 Deletion Syndrome | 15q24 Microdeletion Syndrome | Xq22.3 Deletion Syndrome |
About Prenatal Diagnosis
Prenatal diagnosis refers to the set of instrumental and laboratory investigations through which it is possible to monitor the health and well-being of the fetus during pregnancy.
The use of prenatal diagnostic techniques aims to identify fetal conditions of genetic, infectious, iatrogenic, or environmental origin.
At present, only certain fetal conditions can be detected, but prenatal diagnosis is making great strides forward, allowing us to look to the future with greater possibilities. The various techniques currently available make it possible to detect some multifactorial malformative conditions, chromosomal abnormalities, and genetic diseases for which the specific defect is known, as well as the presence of infectious agents in the genome.
Prenatal diagnostic techniques can be either non-invasive or invasive, depending on whether or not they involve a risk of miscarriage.
Non-invasive methods are procedures that assess the risk of chromosomal abnormalities. They are defined as non-invasive because, being based on ultrasound evaluations and/or maternal blood analysis, they pose no risk to either the mother or the fetus. Their purpose is to detect fetal chromosomal abnormalities, thereby limiting the need for invasive testing. The G-Test® is the most innovative of the non-invasive tests; it is performed on fetal DNA, ensuring both safety and reliability.
Invasive methods involve the collection of tissue samples, through amniocentesis or chorionic villus sampling, with a miscarriage risk ranging between 0.5% and 1%, followed by analysis to determine the presence of genetic abnormalities using different techniques depending on the diagnostic requirements.
About Chromosomal Abnormalities
The human chromosomal set consists of 46 chromosomes organized into 23 distinct pairs. Aneuploidies are abnormalities in chromosome number.
These abnormalities may result in the presence of an additional chromosome (trisomy) or the absence of a chromosome (monosomy). Deletions, on the other hand, occur when a segment of a chromosome is missing, along with the genes located on that chromosomal fragment.
Trisomies
Trisomies are characterized by the presence of an extra chromosome in addition to the normal chromosomal pair. The most common at birth is Trisomy 21, associated with Down syndrome (frequency 1 in 700 live births). Less common are Trisomy 18 (Edwards syndrome, 1 in 7,900), Trisomy 13 (Patau syndrome, 1 in 9,500), Trisomy 22, Trisomy 16, and Trisomy 9, which are even rarer and are usually associated with early miscarriage, intrauterine or perinatal death, or, in any case, very limited life expectancy.
Sex Chromosome Abnormalities
Sex chromosome aneuploidies are characterized by the absence of a sex chromosome, as in Turner syndrome (45,X – frequency 1 in 2,500 females), or by the presence of an extra sex chromosome, as in Klinefelter syndrome (XXY, frequency 1:500 to 1:1,000 males), Jacobs syndrome (XYY, frequency 1 in 1,000 males), and Triple X syndrome (frequency 1 in 1,000 females).
Deletions and Duplications
These are unbalanced chromosomal abnormalities characterized by the absence of a chromosomal segment (or the presence of additional copies of the same fragment) and, consequently, the loss or duplication of the genes located on it. Such alterations cause syndromes of variable clinical significance depending on the chromosome involved, the specific region, and the size of the deleted or duplicated segment.
Some deletions cause rare syndromes, which may be associated with: congenital heart defects, facial dysmorphisms and cleft lip/palate, feeding difficulties in early infancy, gastrointestinal and immune system dysfunctions, intellectual disability, or neurocognitive developmental delay.
At present, these types of chromosomal abnormalities cannot be identified with a traditional karyotype analysis of chorionic villus cells or amniotic fluid.
Main Deletions
-
Cri-du-chat syndrome
-
1p36 deletion syndrome
-
2p33.1 deletion syndrome
-
16p12 deletion syndrome
-
Jacobsen syndrome (11q23 deletion)
-
Prader-Willi/Angelman syndrome (15q11.2)
-
DiGeorge syndrome 2
-
Van der Woude syndrome
Ready to Take the Next Step?
Your journey toward a healthy pregnancy begins with clarity and trusted guidance.
Our team of prenatal specialists and dedicated patient coordinators is here to support you at every stage — from choosing the right test to understanding your results with confidence. We provide gentle, comprehensive assistance designed around the needs of expectant parents.
Schedule a free consultation today and discover how our advanced prenatal and neonatal tests can give you peace of mind and the insights you need for a safe, informed, and reassuring experience.

